This Valentine’s Day I’m pondering the link between birth and our adult loving relationships. A strange link, you might think, but it’s an important one. Our understanding of what psychologists call ‘attachment styles’ – the way we connect with and relate to others (or not) – is that these ways of being with others are created in our early loving connections.
And our early loving connections, in turn, are greatly helped by the cocktail or hormones, particularly the oxytocin ‘love bomb’, that is present during normal physiological child birth.
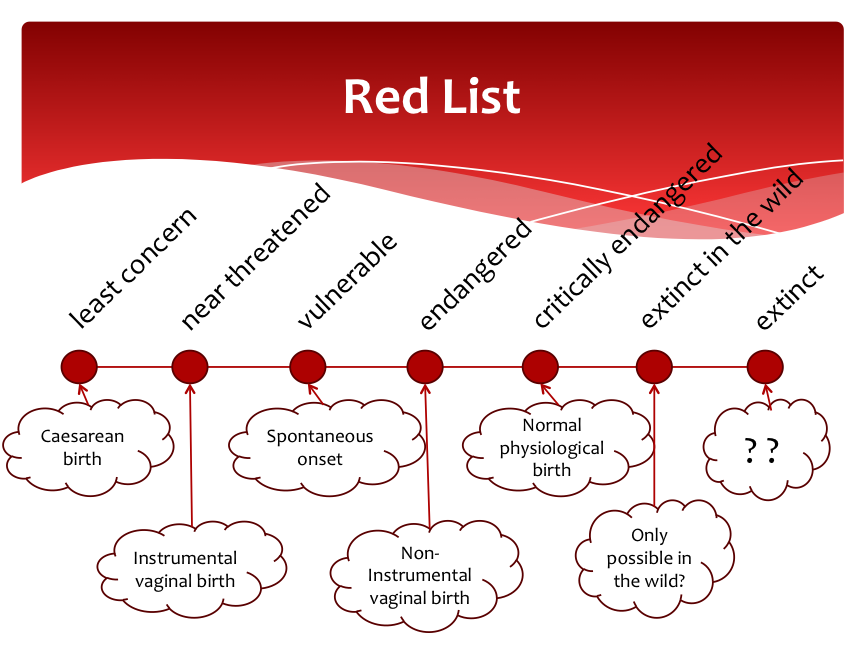
As I say in my book Birth with Confidence, what saddens me about Australia’s unnecessarily high intervention rates is what women and their babies are missing out on. Most women giving birth in Australia today miss out on a naturally unfolding hormone- driven birth—and all the (often downplayed) benefits this kind of birth will bring.
An unintended consequence of our current birth culture is that many births do not end up relying on either the baby’s or the mother’s hormonal input. Ideally in birth, the baby and mother share a connected dance of readiness and response.
Hormonally, the baby triggers the birth, initiating its own birth timing: the mother responds, and their birth dance begins.
In Australia, if we add together the births that use synthetic hormones to artificially kick-start them (induction, 25%) or get the hurry-up (augmentation, 19%) and the babies delivered by ‘elective’ caesarean with no labour at all (18%), then we have 62% of babies definitely not calling the shots on the timing of their births.
Added to this is the huge number of vaginal births in which the final oxytocin surge or ‘love bombing’ in third stage is overridden by an injection of synthetic oxytocin. These intervention rates mean we have a majority of births occurring with neither baby nor mother fully following their own instinctive rhythms or being exposed to the full blast of our evolutionarily programmed love and bonding hormones.
Does it mean anything that the mother and baby are not sharing the hormonal cocktail of normal physiological birth? Does it mean anything that at a societal level so many births occur without any love hormones, let alone the full ‘love bomb’ hormonal cocktail?
Does it matter that in such high numbers of births natural oxytocin is replaced by drips of synthetic oxytocin (which, while able to drive contractions, doesn’t cross the blood-brain barrier and therefore doesn’t initiate bonding behaviours)? That in so many births pethidine and epidural anaesthesia replace natural endorphins and intense human support? That synthetic oxytocin delivers the placenta, replacing the surge of natural oxytocin that facilitates bonding and loving connections?
Well, social anthropologists, physiology researchers and neuro- biologists say it means a lot. And so do many of the mothers who have unwittingly ended up with one of these ‘no love hormone’ births. Much of the new discipline of neurobiology takes as its basic premise the importance of our species’ need for social connectedness (read oxytocin) and empathy. In other words—love. They don’t specifically look at what happens during birth, but they do look at the earliest interactions of babies with their carers, generally mothers. They take as their starting point this early infant period and the absolute need for the human infant to be securely attached to nurturing caregivers for its ongoing physical, mental and relational ‘thriving’. They know that the quality of our early interactions and nurturing (or not) affect our biology.
So if, in our era of high interventions, we so regularly interfere with the physiological, biological basis of the capacity for early bonded interactions in both the mother and the baby … what might be the implications?
This is what I find myself pondering on this day that celebrates love. I hope your Valentine’s Day is full of that ‘tend and befriend’ oxytocin hormone. And I hope too, that our birth culture will get much better at allowing the wonderful hormonal cocktail that comes with normal birth to unfold for birthing women to come.





 Birth with Confidence: savvy choices for normal birth
Birth with Confidence: savvy choices for normal birth